Weather impact on airborne coronavirus survival: Physics of Fluids: Vol 32, No 9
ABSTRACT
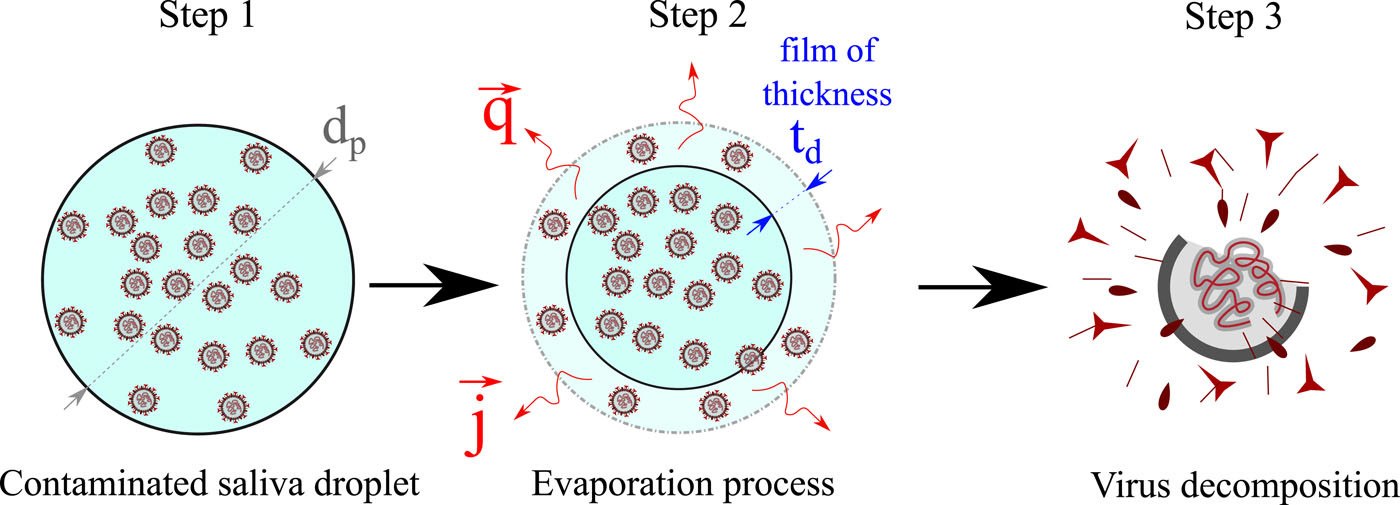
The contribution of this paper toward understanding of airborne coronavirus survival is twofold: We develop new theoretical correlations for the unsteady evaporation of coronavirus (CoV) contaminated saliva droplets. Furthermore, we implement the new correlations in a three-dimensional multiphase Eulerian–Lagrangian computational fluid dynamics solver to study the effects of weather conditions on airborne virus transmission. The new theory introduces a thermal history kernel and provides transient Nusselt (Nu) and Sherwood (Sh) numbers as a function of the Reynolds (Re), Prandtl (Pr), and Schmidt numbers (Sc). For the first time, these new correlations take into account the mixture properties due to the concentration of CoV particles in a saliva droplet. We show that the steady-state relationships induce significant errors and must not be applied in unsteady saliva droplet evaporation. The classical theory introduces substantial deviations in Nu and Sh values when increasing the Reynolds number defined at the droplet scale. The effects of relative humidity, temperature, and wind speed on the transport and viability of CoV in a cloud of airborne saliva droplets are also examined. The results reveal that a significant reduction of virus viability occurs when both high temperature and low relative humidity occur. The droplet cloud’s traveled distance and concentration remain significant at any temperature if the relative humidity is high, which is in contradiction with what was previously believed by many epidemiologists. The above could explain the increase in CoV cases in many crowded cities around the middle of July (e.g., Delhi), where both high temperature and high relative humidity values were recorded one month earlier (during June). Moreover, it creates a crucial alert for the possibility of a second wave of the pandemic in the coming autumn and winter seasons when low temperatures and high wind speeds will increase airborne virus survival and transmission.
ACKNOWLEDGMENTS
The authors would like to thank the Editor-in-Chief and Physics of Fluids staff for their assistance during the peer-review and publication of this manuscript.
REFERENCES
- M. Richard, J. van den Brand, T. Bestebroer, P. Lexmond, D. de Meulder, R. Fouchier, A. Lowen, and S. Herfst, “Influenza a viruses are transmitted via the air from the nasal respiratory epithelium of ferrets,” Nat. Commun. 11, 766 (2020). https://doi.org/10.1038/s41467-020-14626-0, Google ScholarCrossref
- Z. Lei, Q. Yuhang, L.-F. Paolo, C. Yi, and Z. Yangying, “COVID-19: Effects of weather conditions on the propagation of respiratory droplets,” medRxiv (2020). https://doi.org/10.1101/2020.05.24.20111963, Google ScholarCrossref
- R. Zhang, Y. Li, A. L. Zhang, Y. Wang, and M. J. Molina, “Identifying airborne transmission as the dominant route for the spread of COVID-19,” Proc. Natl. Acad. Sci. U. S. A. 117, 14857–14863 (2020). https://doi.org/10.1073/pnas.2009637117, Google ScholarCrossref
- C. B. Beggs, “The airborne transmission of infection in hospital buildings: Fact or fiction?,” Indoor Built Environ. 12, 9–18 (2003). https://doi.org/10.1177/1420326×03012001002, Google ScholarCrossref
- B. Killingley and J. Nguyen-Van-Tam, “Routes of influenza transmission,” Influenza Other Respir. Viruses 7, 42–51 (2013). https://doi.org/10.1111/irv.12080, Google ScholarCrossref
- R. E. Davis, C. E. Rossier, and K. B. Enfield, “The impact of weather on influenza and pneumonia mortality in New York city, 1975–2002: A retrospective study,” PLoS One 7, e34091 (2012). https://doi.org/10.1371/journal.pone.0034091, Google ScholarCrossref
- K. M. Gustin, J. A. Belser, V. Veguilla, H. Zeng, J. M. Katz, T. M. Tumpey, and T. R. Maines, “Environmental conditions affect exhalation of h3n2 seasonal and variant influenza viruses and respiratory droplet transmission in ferrets,” PLoS One 10, e0125874 (2015). https://doi.org/10.1371/journal.pone.0125874, Google ScholarCrossref
- D. Zang, S. Tarafdar, Y. Yu. Tarasevich, M. Dutta Choudhury, and T. Dutta, “Evaporation of a droplet: From physics to applications,” Phys. Rep. 804, 1–56 (2019). https://doi.org/10.1016/j.physrep.2019.01.008, Google ScholarCrossref
- S. S. Sazhin, “Advanced models of fuel droplet heating and evaporation,” Prog. Energy Combust. Sci. 32, 162–214 (2006). https://doi.org/10.1016/j.pecs.2005.11.001, Google ScholarCrossref
- E. P. Vejerano and L. C. Marr, “Physico-chemical characteristics of evaporating respiratory fluid droplets,” J. R. Soc. Interface 15, 20170939 (2018). https://doi.org/10.1098/rsif.2017.0939, Google ScholarCrossref
- W. E. Ranz and W. R. Marshall, “Evaporation from drops, Part I,” Chem. Eng. Prog. 48, 141–146 (1952). Google Scholar
- W. E. Ranz and W. R. Marshall, “Evaporation from drops, Part II,” Chem. Eng. Prog. 48, 173–180 (1952). Google Scholar
- P. Mecenas, R. Bastos, A. Vallinoto, and D. Normando, “Effects of temperature and humidity on the spread of COVID-19: A systematic review.” medRxiv:20064923 (2020). Google Scholar
- Q. Li, X. Guan, P. Wu, X. Wang, L. Zhou et al., “Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia,” N. Engl. J. Med. 382(13), 1199–1207 (2020). https://doi.org/10.1056/NEJMoa2001316, Google ScholarCrossref
- C. I. Paules, H. D. Marston, and A. S. Fauci, “Coronavirus infections-more than just the common cold,” JAMA 323, 707–708 (2020). https://doi.org/10.1001/jama.2020.0757, Google ScholarCrossref
- M. Moriyama, W. Hugentobler, and A. Iwasaki, “Seasonality of respiratory viral infections,” Annu. Rev. Virol. 7, 2.1–2.19 (2020). https://doi.org/10.1146/annurev-virology-012420-022445, Google ScholarCrossref
- R. Bhardwaj and A. Agrawal, “Tailoring surface wettability to reduce chances of infection of COVID-19 by a respiratory droplet and to improve the effectiveness of personal protection equipment,” Phys. Fluids 32, 081702 (2020). https://doi.org/10.1063/5.0020249, Google ScholarScitation, ISI
- R. Bhardwaj and A. Agrawal, “Likelihood of survival of coronavirus in a respiratory droplet deposited on a solid surface,” Phys. Fluids 32, 061704 (2020). https://doi.org/10.1063/5.0012009, Google ScholarScitation, ISI
- K. H. Chan, J. S. Malik Peiris, S. Y. Lam, L. L. M. Poon, K. Y. Yuen, and W. H. Seto, “The effects of temperature and relative humidity on the viability of the SARS coronavirus.” Adv Virol. 2011, 1–7. https://doi.org/10.1155/2011/734690, Google ScholarCrossref
- K. K.-W. To, O. T.-Y. Tsang, C. C.-Y. Yip, K.-H. Chan, T.-C. Wu, J. M.-C. Chan, W.-S. Leung, T. S.-H. Chik, C. Y.-C. Choi, D. H. Kandamby, D. C. Lung, A. R. Tam, R. W.-S. Poon, A. Y.-F. Fung, I. F.-N. Hung, V. C.-C. Cheng, J. F.-W. Chan, and K.-Y. Yuen, “Consistent detection of 2019 novel coronavirus in saliva,” Clin. Infect. Dis. 71, 841–843 (2020). https://doi.org/10.1093/cid/ciaa149, Google ScholarCrossref
- R. Xu, B. Cui, X. Duan, P. Zhang, X. Zhou, and Q. Yuan, “Saliva: Potential diagnostic value and transmission of 2019-nCov,” Int. J. Oral Sci. 12, 1–6 (2020). https://doi.org/10.1038/s41368-020-0080-z, Google ScholarCrossref
- N. L’Helgouach, P. Champigneux, F. Santos-Schneider, L. Molina, J. Espeut, M. Alali, J. Baptiste, L. Cardeur, B. Dubuc, V. Foulongne, F. Galtier, A. Makinson, G. Marin, M.-C. Picot, A. Prieux-Lejeune, M. Quenot, F. J. Checa-Robles, N. Salvetat, D. Vetter, J. Reynes, and F. Molina, “EasyCOV : Lamp based rapid detection of SARS-COV-2 in saliva,” medRxiv:20117291 (2020). Google Scholar
- L. Azzi, G. Carcano, F. Gianfagna, P. Grossi, D. D. Gasperina, A. Genoni, M. Fasano, F. Sessa, L. Tettamanti, F. Carinci, V. Maurino, A. Rossi, A. Tagliabue, and A. Baj, “Salivais a reliable tool to detect SARS-CoV-2,” J. Infect. 81, e45–e50 (2020). https://doi.org/10.1016/j.jinf.2020.04.005, Google ScholarCrossref
- J. H. Azzolini, K. C. Winkler, and S. M. Kool, “Virus survival as a seasonal factor in influenza and poliomyelitis,” Nature 188, 430–431 (1960). https://doi.org/10.1038/188430a0, Google ScholarCrossref
- J. Shaman, M. Kohn, and B. H. Singer, “Absolute humidity modulates influenza survival, transmission, and seasonality,” Proc. Natl. Acad. Sci. U. S. A. 106, 3243–3248 (2009). https://doi.org/10.1073/pnas.0806852106, Google ScholarCrossref
- J. Shaman, E. Goldstein, and M. Lipsitch, “Absolute humidity and pandemic versus epidemic influenza,” Am. J. Epidemiol. 173, 127–135 (2011). https://doi.org/10.1093/aje/kwq347, Google ScholarCrossref
- T. Myatt, M. Kaufman, J. Allen, D. MacIntosh, M. Fabian, and J. McDevitt, “Modeling the airborne survival of influenza virus in a residential setting: The impacts of home humidification,” Environ. Health 9, 55 (2010). https://doi.org/10.1186/1476-069X-9-55, Google ScholarCrossref
- W. Yang and L. Marr, “Mechanisms by which ambient humidity may affect viruses in aerosols,” Appl. Environ. Microbiol. 78, 6781–6788 (2012). https://doi.org/10.1128/AEM.01658-12, Google ScholarCrossref
- M. Sobsey and J. Meschke, “Virus survival in the environment with special attention to survival in sewage droplets and other environmental media of fecal or respiratory origin.” Res. Gate 1-71, 22855142 (2003). Google Scholar
- G. J. Harper, “Airborne micro-organisms: Survival tests with four viruses,” Epidemiol. Infect. 59(4), 479–486 (1961). https://doi.org/10.1017/s0022172400039176, Google ScholarCrossref
- S. J. Webb, R. Bather, and R. W. Hodges, “The effect of relative humidity and inositol on air-borne viruses,” Can. J. Microbiol. 9, 87–92 (1963). https://doi.org/10.1139/m63-009, Google ScholarCrossref
- T. Dbouk and D. Drikakis, “On coughing and airborne droplet transmission to humans,” Phys. Fluids 32, 053310 (2020). https://doi.org/10.1063/5.0011960, Google ScholarScitation, ISI
- I. B. Celik, U. Ghia, P. J. Roache, and C. J. Freitas, “Procedure for estimation and reporting of uncertainty due to discretization in CFD applications,” J. Fluids Eng. 130, 078001 (2008). https://doi.org/10.1115/1.2960953, Google ScholarCrossref
- F. Moukalled, L. Mangani, and M. Darwish, The Finite Volume Method in Computational Fluid Dynamics: An Advanced Introduction with OpenFOAM and Matlab, 1st ed. (Springer Publishing Company, Incorporated, 2015). Google Scholar
- T. Miyoshi, M. Lönnfors, J. Peter Slotte, and S. Kato, “A detailed analysis of partial molecular volumes in DPPC/cholesterol binary bilayers,” Biochim. Biophys. Acta (BBA) 1838, 3069–3077 (2014). https://doi.org/10.1016/j.bbamem.2014.07.004, Google ScholarCrossref
- C. Hidalgo, Physical Properties of Biological Membranes and Their Functional Implications (Plenum press, New York, London, 1988). Google ScholarCrossref
- S. Youssefian, N. Rahbar, C. R. Lambert, and S. Van Dessel., “Variation of thermal conductivity of DPPC lipid bilayer membranes around the phase transition temperature,” R. Soc. Interface 14, 20170127 (2017). https://doi.org/10.1098/rsif.2017.0127, Google ScholarCrossref
- W. Fuchs, “Z. d. sowj.-union6,” Physik 224 S (1934). Google Scholar
- W. F. Wells, “On air-borne infection: Study II. Droplets and droplet nuclei,” Am. J. Hyg. 20, 611–618 (1934). https://doi.org/10.1093/oxfordjournals.aje.a118097, Google ScholarCrossref
- N. Frossling, “Uber die verdunstung fallender tropfen (the evaporation of falling drops),” Gerlands Beitrage Geophys. 52 (1938). Google Scholar
- A. Acrivos and T. D. Taylor, “Heat and mass transfer from single spheres in Stokes flow,” Phys. Fluids 5, 387–394 (1962). https://doi.org/10.1063/1.1706630, Google ScholarScitation, ISI
- H. Brenner, “Forced convection heat and mass transfer at small Péclet numbers from a particle of arbitrary shape,” Chem. Eng. Sci. 18, 109–122 (1963). https://doi.org/10.1016/0009-2509(63)80020-2, Google ScholarCrossref
- P. D. Richardson, WADD 59-1, 1968. Google Scholar
- S. Whitaker, “Forced convection heat transfer correlations for flow in pipes, past flat plates, single cylinders, single spheres, and for flow in packed beds and tube bundles,” AIChE J. 18, 361–371 (1972). https://doi.org/10.1002/aic.690180219, Google ScholarCrossref
- H. Kramers, “Heat transfer from spheres to flowing media,” Physica 12, 61–80 (1946). https://doi.org/10.1016/S0031-8914(46)80024-7, Google ScholarCrossref
- C. Vliet and J. C. Leppert, “Closure to “discussions of ‘forced convection heat transfer from an isothermal sphere to water’” (1961, ASME J. Heat Transfer, 83, pp. 170–175),” J. Heat Trarnsfer 83, 170–175 (1961). https://doi.org/10.1115/1.3680509, Google ScholarCrossref
- Z.-G. Feng and E. E. Michaelides, “Unsteady heat transfer from a sphere at small Péclet numbers,” J. Fluid Eng. 118, 96–102 (1996). https://doi.org/10.1115/1.2817522, Google ScholarCrossref
- Z.-G. Feng and E. E. Michaelides, “Transient heat transfer from a particle with arbitrary shape and motion,” J. Heat Transfer 120, 674–681 (1998). https://doi.org/10.1115/1.2824336, Google ScholarCrossref
- Z.-G. Feng and E. E. Michaelides, “A numerical study on the transient heat transfer from a sphere at high Reynolds and Péclet numbers,” Int. J. Heat Mass Transfer 43, 219–229 (2000). https://doi.org/10.1016/s0017-9310(99)00133-7, Google ScholarCrossref
- Z.-G. Feng and E. E. Michaelides, “Heat and mass transfer coefficients of viscous spheres,” Int. J. Heat Mass Transfer 44, 4445–4454 (2001). https://doi.org/10.1016/s0017-9310(01)00090-4, Google ScholarCrossref
- Z. Duan, B. He, and Y. Duan, “Sphere drag and heat transfer,” Sci. Rep. 5, 1–7 (2015). https://doi.org/10.1038/srep12304, Google ScholarCrossref
- P. Yearling and R. Gould, Convective Heat and Mass Transfer from Single Evaporating Water, Methanol and Ethanol Droplets (American Society of Mechanical Engineers, New York, NY, USA, 1995). Google Scholar
- E. Pfender, “Heat and momentum transfer to particles in thermal plasma flows,” Pure Appl. Chem. 57(9), 1179–1195 (1985). https://doi.org/10.1351/pac198557091179, Google ScholarCrossref
- T. H. Chilton and A. Colburn, “Mass transfer (absorption) coefficients prediction from data on heat transfer and fluid friction,” Ind. Eng. Chem. 26, 1183–1187 (1934). https://doi.org/10.1021/ie50299a012, Google ScholarCrossref
- E. Pohlhausen, “Der wärmeaustausch zwischen festen körpern und flüssigkeiten mit kleiner reibung und kleiner wärmeleitung,” ZAMM-J. Angew. Math Mech. 1, 115–121 (1921). https://doi.org/10.1002/zamm.19210010205, Google ScholarCrossref
- T. Dbouk and D. Drikakis, “On respiratory droplets and face masks,” Phys. Fluids 32, 063303 (2020). https://doi.org/10.1063/5.0015044, Google ScholarScitation, ISI
- V. Vinoj, N. Gopinath, K. Landu, B. Behera, and B. Mishra, “The COVID-19 spread in India and its dependence on temperature and relative humidity,” arXiv:2020070082 (2020). Google Scholar
Published under license by AIP Publishing.
You can read the full paper here